On logistic regression versus support vectors machine using vaccination dataset
Keywords:
Logistic regression, Leave out-one validation, Support vectors machine, Prediction, VaccinationAbstract
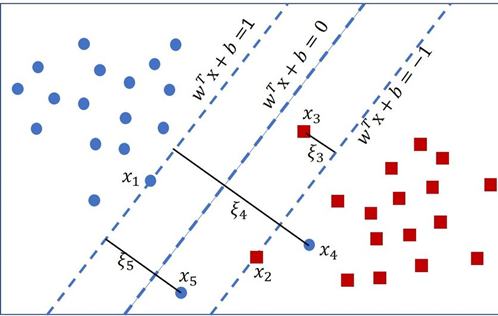
The performance of two classification techniques, logistic regression and Support Vector Machines (SVMs), in assessing vaccination data is investigated in this study. The model was trained based on leave-out-one cross validation to obtain an accurate result. Simulated with ten thousand replications, a life data set was used to establish a better model. The findings from the simulation revealed that the logistic regression model slightly outperformed the SVM while the life data shows that the tuned SVM outperformed both the logistic and the SVM. This demonstrates the practical utility of advanced approaches such as SVMs in difficult categorization scenarios such as vaccination prediction. The study emphasizes the superiority of the customized SVM model in this setting, as well as the potential of machine learning approaches to increase comprehension of complicated healthcare scenarios and guide data-driven decision-making for influencing vaccination plans and public health. The study recommends the use of logistic regression if the data point is high.
Published
How to Cite
Issue
Section
Copyright (c) 2023 Olumide S. Adesina, Adedayo F. Adedotuun, Kayode S. Adekeye, Ogbu F. Imaga, Adeleke J. Adeyiga, Toluwalase J. Akingbade

This work is licensed under a Creative Commons Attribution 4.0 International License.